You are not alone with your back pain. Eight out of ten adults will experience back pain in their lifetime, and it is also very common for episodes of back pain to recur from time to time. Despite this, most will be able to continue their usual pastimes and work.
In this page you can find information on back pain and its treatment. You will get information on how you can shorten the periods of pain and influence the recurrence of such events. Most of the pains will heal on their own and have a good prognosis. Sometimes, however, back symptoms may recur or persist, in which case you will be able to cope better with your back pain by following the instructions here.
You can jump directly to the section you want by using the table of contents below.

Photo: iStock
Back structure
The spine is the supporting structure of the body that protects the spinal cord that runs within it. The spine is made up of vertebrae, between which there are discs. The outer circumference of a disc is made of dense fibrous cartilage tissue and its inner part comprises a jelly-like mass. The intervertebral discs are like cushions that act as shock absorbers and allow the spine to move. In addition to the discs, the vertebrae of the spine are connected to each other by means of facet joints. The function of facet joints is to stabilize the movements of the spine.
Strong and flexible muscles support the spine formed by vertebrae and discs. Sufficient body muscle strength is important for the functioning of the back and reduces the loads placed on the back.
As we age, our body undergoes normal changes, for example, wrinkles form on the skin. The spine also undergoes natural changes related to aging: the discs dry out and shrink, whilst vertebrae move closer to each other. Changes to the structures start to occur at a young age, although these changes are usually unrelated to back pain.

Photo: Dreamstime
Back pain
Lower back symptoms, such as pain, muscle tension or stiffness, are localized between the lowest ribs and the gluteal folds. The symptoms may be accompanied by pain reflected in one or both of the lower limbs. Often, symptoms reflected in a lower limb are radiation sensations from the structures of the lower back, and there is no nerve irritation behind them. If there is nerve root irritation from the spine, it may cause nerve-related symptoms, such as lower limb pain, numbness, insensitivity, tingling and muscle weakness.

Pain can be classified according to its duration.
Acute or sudden pain lasts from a few days to several, about six (6), weeks. The pain is considered to be prolonged when it lasts for 6–12 weeks. Pain lasting more than 12 weeks is classified as being chronic.
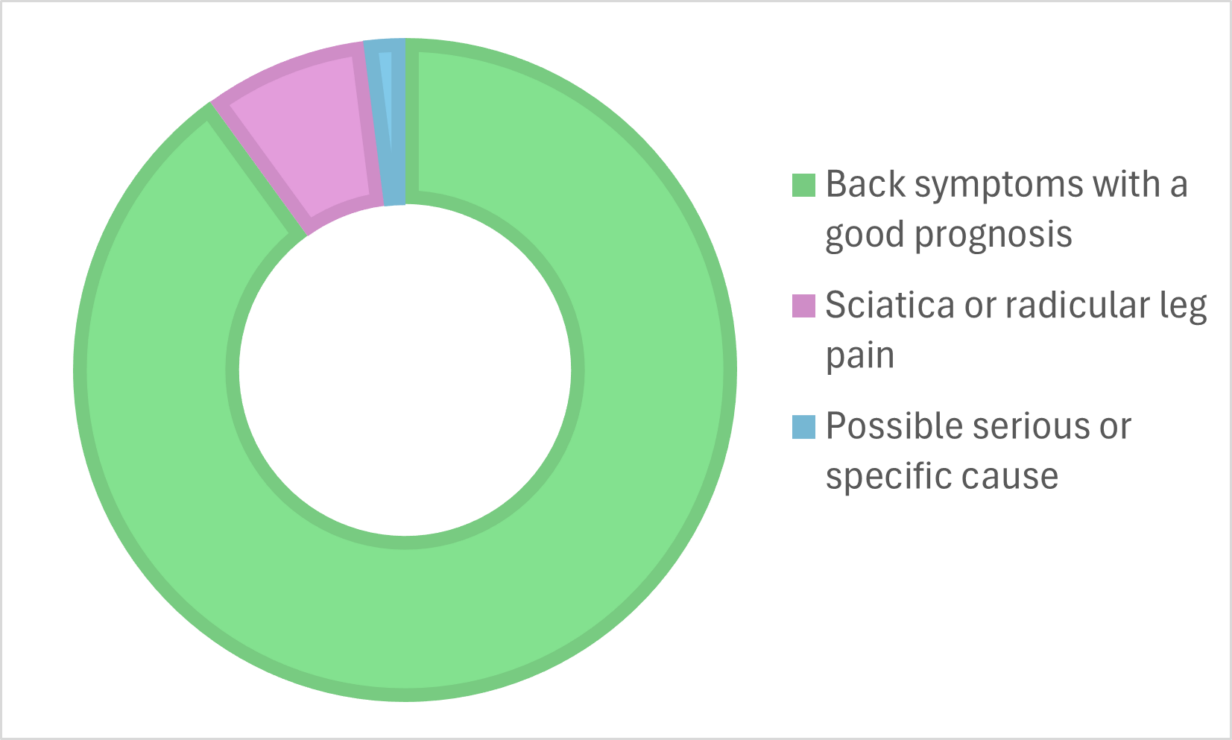
Lower back pain is divided into three groups based on the symptoms.
- Back symptoms with a good prognosis: these account for almost 90 percent of back pains. If a doctor’s examination shows no signs of serious diseases and no sciatica symptoms occur, the symptom is classified as lower back pain with a good prognosis. An exact anatomical diagnosis is then neither possible nor necessary. Often this kind of back pain is caused by small tissue damage in the tissues surrounding the spine, such as a slipped intervertebral disc or a sprained muscle or ligament. Sudden-onset soft-tissue sprains are often called lumbago. The symptoms typically appear in the back and pelvis area.
- Radicular leg pain (sciatica): lower limb symptoms suggest nerve root dysfunction, the cause of which is often irritation or compression of the nerve root leaving the spinal cord. Most of these resolve on their own within three months.
- A possible serious or specific cause, which comprises only a few percent of all back symptoms.
In connection with back symptoms, it is important to recognize factors that may slow down the healing process. The factors listed below may affect the interpretation of the pain and the prolongation of the pain:
- the belief that pain and activity (for example, movement and work) would be harmful
- excessive bed rest
- overcaution and fear of pain and injury that limit movement
- low mood, anxiety and social withdrawal
- problems at work and dissatisfaction with work
- an over-caring family or lack of support
- the seeking of many different treatments
- receiving negative, frightening or incorrect information about back pain.
What factors contribute to back pain?
Although there are several suspected risk factors for back pain, there is no strong research data on the causal relationship of any factor. It is, however, known that the factors predicting long-term disabling lower back pain include genetic factors, the severity and extent of the symptoms (e.g., multi-site pain), lifestyle factors (e.g., sleep disorders), multimorbidity (especially asthma, headache, diabetes and mental health problems), social factors (a low socio-economic status, unemployment, work-related factors) and psychological factors (such as depression, anxiety and low self-efficacy). Being both overweight and smoking will also increase the risk of prolonged back pain.
Back health and well-being are supported by general health-promoting lifestyles, such as regular exercise, a healthy diet and sufficient sleep. Exercise and movement also contribute to shortening episodes of pain and reducing their recurrence. Attention should also be paid to lifestyles and the well-being of the back already in children and young people.
The psychological and social load of work can affect the prolongation and discomfort of back pain. A lack of opportunities to have an influence, stress, a bad work atmosphere and lack of support at work can increase back symptoms. The physical load of the work may also contribute to the prolongation of back pain, if the work involves repeated forward bending, long-lasting work when in the same position, twisted positions, loads that are difficult to lift, or work routines that require one to stand still for an extended time. In addition to the employee themself, occupational health care, the employer and the work community also play a key role in preventing the prolongation of back pain and supporting the ability to work. There is no need to persevere with back symptoms for too long: if the symptoms hinder your work, you should contact occupational health care.

Photo: iStock
When should you be examined?
Back pain often gets better on its own, and a visit to the doctor is not always necessary. If you experience the following symptoms, you should, however, see a doctor:
- The back pain is very strong and/or sudden.
- The pain is unbearable and no position can be found that allows it to ease up.
- Coping with daily tasks is hindered or limited.
- The back pain is accompanied by fever or a deterioration in general well-being.
- The back pain is linked to an accident.
- You have or have had cancer in the past.
If the back pain is accompanied by difficulty starting to urinate or disturbances in the ability to hold urine or faeces, numbness in the anus area, or progressive weakness of the muscles of the foot, you should go to the hospital immediately.
With frequent and prolonged back pain, a good patient-doctor relationship is important. When you visit the same doctor, he or she will gain a good overall understanding of your back pain. Your doctor will also be able to best assess the necessity of any examinations and treatments.
Back symptoms in health care
If the back pain does not subside on its own or the episodes of back pain recur frequently, you can seek a direct access appointment with a physiotherapist. Direct access to a physiotherapist means that a person with back symptoms can seek a physiotherapist’s appointment without first seeing a doctor. When you are in contact with primary or occupational health care, a nurse trained for the task will make an assessment as to whether you should be referred to a physiotherapist or a doctor. Through a direct access appointment, the physiotherapist can examine, give advice and guidance, and make a follow-up action plan with the client. If necessary, the physiotherapist can also refer you to a GP or occupational health physician.
The task of the doctor is to rule out harmful diseases or to diagnose diseases that require specific treatment. At the appointment, the doctor will assess the need for further tests and monitor the patient, and agree on a possible check-up appointment. Based on the examination results and the development of the symptom picture, the doctor will, if necessary, make a referral to specialist medical care and/or consult a specialist (e.g., a physiatrist, rheumatologist or orthopaedist) in non-urgent situations affecting the ability to work.
If your pain persists
In the case of long-lasting and challenging back pain, your doctor may send you to a rehabilitation or pain outpatient clinic for specialized medical care. There, in a multiprofessional treatment team, other professionals, such as a physiotherapist, psychologist and social worker, depending on your situation, may participate in the examinations and treatment in addition to the specialist doctor(s).

Photo: Pexels
How an examination proceeds?
Interview
The doctor and physiotherapist will find out more by asking questions about things related to your back pain, such as your life situation, the performance of everyday tasks, other diseases, weight changes and medications in use. Because of this, several questions may be asked at the reception: what kind of symptoms you have, whether the symptoms started gradually or suddenly following an injury, what eases the symptoms and what makes them worse. You can prepare to answer these questions prior to coming to the appointment.
Clinical examination
The examination usually starts of by looking at the position of the back and the use of the back and general movement, such as walking. In addition, the mobility of the spine is examined. After that, the muscle strength of the back and lower limbs, the feeling of the lower limbs and tendon reflexes are usually examined.
Other examinations:
If the back pain is accompanied by sciatica pain radiating to a lower limb and the doctor notes changes in muscle strength, tendon reflexes and sensations, additional examinations are often needed to determine the cause and treatment of the back pain (MRI, i.e., magnetic resonance imaging or ENMG, i.e., nerve path examination). It is worthwhile noting that, for example, an MRI scan of the spine may reveal aging-related changes that are not the cause of the pain.
The underlying cause of back pain is usually not visible on imaging. Imaging is used if, based on the symptoms and examination, a suspicion of a serious or specific back disease arises. Imaging is often used as a research aid in confirming a diagnosis or as an exclusion test.
Medication
Painkillers relieve symptoms, help with everyday life and movement, and ensure adequate sleep. Paracetamol is usually the preferred self-medication option and a maximum of 3,000 mg/day of paracetamol may be taken. This daily dose must not be exceeded.
Over-the-counter anti-inflammatory drugs such as ibuprofen may also be used for acute back pain. They relieve pain and calm inflammatory reactions. It must be noted that two different anti-inflammatory medications should not be used at the same time, and the dosing instructions on the packages must be followed.
For pain that hinders your ability to function, you should use a painkiller that is suitable for you (paracetamol and/or an anti-inflammatory) at the maximum dose for two to three days or, if necessary, for 5–7 days. This can help you to move, function in everyday life, work and sleep. Use pain medication for short periods of time: it is not advisable to take medicine just to be on the “safe side”.
Once the pain is relieved, you can restore blood circulation to the tight muscles through movements. This way it may be possible to shorten the duration of the pain period.
If the back pain is severe, you may require painkillers that are only prescribed by a doctor. These are usually either anti-inflammatory medications or muscle relaxants. Opioid drugs may have to be used infrequently and for a short time. These drugs may be offered to use in severe nerve root pain or post-surgery pain.
Medications that raise the pain threshold (tricyclic antidepressants at a low dose), antiepileptics gabapentin and pregabalin, and pain-relieving antidepressants are offered for nerve damage pain and chronic pain.
Please note that, for example, underlying diseases or other medication may affect the suitability of painkillers. Talk to your doctor about the benefits and harms of medications.

Photo: Pexels
Surgical treatment
There must always be a clear basis for a surgery to take place. Not even severe localized back pain requires surgical treatment, if no clear reason for surgery has been found in the examinations. If you have experienced disturbing, radiating pain in a lower limb for more than six weeks and you have clinical signs of nerve root compression, you can talk to your doctor about further treatment and also possible surgical treatment.
Surgical treatment is deemed to be necessary if severe nerve root or spinal canal stenosis is accompanied by difficulty starting to urinate or disturbances in the ability to hold urine or faeces, a progressive weakening of the strength of the extensor or flexor muscles of the foot or the thigh muscle, as well as intolerable pain radiating to a lower limb that is not sufficiently relieved even by strong painkillers.
Before a possible surgery, the operating doctor will tell you more about the planned procedure, the expected benefits, and possible complications and risks. After a surgery, active rehabilitation is important in order to restore functional abilities.

Photo: Shutterstock
What can you do yourself?
You can influence your back symptoms through self-care. Think about what worsens your back symptoms and what you can do to ease them. You can also seek support for self-care from healthcare professionals. The most important goal is to continue your daily activities at work and in your free time as well as possible. Remember that a short bed rest, even one that lasts only a couple of days, will slow down the recovery from back pain.
Exercise
In the early stages of a period of pain, you can promote the recovery process through exercise, such as light everyday chores. Once the worst period of pain has eased, you can gradually increase your movement.
You can try the following to increase movement:
- Walk (with or without Nordic walking poles) for short distances one or a few times a day.
- Engage in light home training and incidental activity.
- Perform movements in water, such as swimming, or go cycling.

Photo: Unsplash
As the back pain is alleviated, functional limitations will also decrease. Gradually increase the duration, frequency and intensity of movements. The symptoms may sometimes increase a little at the beginning, but this is no reason to worry. If the pain gets worse, talk to your doctor.
Back symptoms maybe sometimes be prolonged. In such a case, it is worthwhile visiting, e.g., a physiotherapist’s office in order to receive exercise instructions. Voluntary exercise is also beneficial. With prolonged lower back pain, exercise often decreases the pain and the recurrence of episodes of pain and improves functional and work capacity.
With back pain that has lasted for a long time (more than 12 weeks), regular training and exercise are the most effective forms of treatment. By ensuring sufficient exercise and diverse use of your back, you can prevent or reduce the pain yourself. Exercise and training are also beneficial in recovering from surgery.
It is essential to move despite any moderate pain, as it often helps to speed up the recovery process. By trying out different sports and forms of exercise, you will be able to find suitable ways to improve your overall fitness and promote the well-being of your back.
Exercise instructions in image and video format (in Finnish).

Photo: Shutterstock
Sleep, stress and recovery
Get enough sleep. Sleep is important for the recovery of both brain and body functions. Sleep problems sensitize you to pain and poor sleep can lead to a situation in which the pain regulation system is disturbed and the pain threshold is lowered, which will lead to increased sensitization to pain.
You can influence the quality and quantity of your sleep. Medicinal-free treatment is initially recommended for insomnia, and you can try the following ways to sleep better:
- Aim for regular bedtimes and wake-ups. A few hours before going to sleep, avoid bright lights and loud noises, calm down your evening.
- Try relaxation exercises. In case of back pain, back rest and relaxation positions can ease the symptoms and help the body to relax.
- Avoid caffeine and alcohol.

Photo: Pexels
Among other things, stress and worries directly affect sleep rhythms and the quantity and quality of sleep. Stress factors may also predispose one to pain. Stress may be caused by various difficulties in a life situation, and burdensome experiences experienced in the past also predispose individuals to it. Prolonged pain is always accompanied by some degree of stress.
In terms of pain management, it is also beneficial if you can accept the pain in some way. It will reduce stress levels, and allow you to cope better over time. Such acceptance does not mean giving up the hope of recovery or the right to receive good pain treatment.
You can try the following ways to affect stress levels:
- Find ways to relax. Relaxation relieves muscle tension, decreasing the stress caused by a pain condition and, consequently, reduces the pain.
- Try breathing exercises. They calm and lengthen the breathing rhythm. Deep and calm breathing is one of the most important mechanisms for relaxation.
- You can try a conscious presence exercises. Noticing and accepting one’s body sensations reduces feelings of tension.
- Return to pleasant things and hobbies both in your imagination and in practice.
- Be your own best friend – you don’t have to expect too much from yourself. Treat yourself with compassion.
- Have a positive attitude towards social situations. Pain makes many people withdraw, whilst socializing can reduce feelings of loneliness and stress.
- Exercise and healthy nutrition help recovery and tolerance to stress.

Photo: Pexels
Other self-care remedies
Cold and heat treatment
In the acute phase of back pain, you can try placing a cold pack on the painful area for 10–20 minutes. Put a thin towel between the skin and the cold pack. Heat therapy can reduce sudden and prolonged back pain in the short term. You can get a heat pack and heat it according to the instructions. A heating pad or a heated bag of oats will also work. Apply heat for about 15–20 minutes.
Both heat and cold treatment can be repeated several times a day and be combined with, e.g., back rest and relaxation positions. In addition to heat and cold therapy, you should continue your usual daily activities at work and in your free time.
TENS treatment
TENS treatment, i.e., so-called transcutaneous nerve stimulation, is based on low-power electrical stimulation transmitted through the skin. Low-frequency electrical impulses are used to activate pain-relieving mechanisms. TENS treatment can be used to relieve back pain not only when at rest, but also when moving, such as during walking. It can promote the start of movement and facilitate movement by reducing associated pain sensations.
Back brace
There is no research evidence that supports the use of back brace in preventing lower back pain or its recurrence. However, some people with back problems find that a back brace makes it easier to move by reducing muscle tension in the area of pain.

Photo: Pexels
What to remember in everyday life and at work
- Vary your working positions and, if possible, use workstation adjustments in a variety of ways.
- Take regular breaks from long periods of continuous standing still. Walk around or do other exercises during the workday or while traveling. Also perform movements in the opposite direction to your main working position.
- If your job involves awkward working positions and handling heavy loads, it is worthwhile discussing at the workplace how the loads could be reduced until the back symptoms calm down. Remember that it is possible to cope with back pain, even in physically demanding work.
- Talk to the occupational health care and your supervisor about how you could continue working despite the back pain.

Photo: iStock
Good to remember
- In most cases, back pain only lasts for a short time and the symptoms are relieved without a visit to the doctor.
- Back pain rarely means that there is serious damage to the back.
- Increase the number of things you do a little at a time. As the back pain eases, functional limitations will also decrease.
- During the night, the body recovers from the stresses of the day. When sleeping, healthy discs fill up with fluid. Therefore, when you wake up in the morning, your back may feel stiff for the first few hours. Sufficient sleep is important for the well-being of the back.
- Daily exercise strengthens the body’s own pain regulation systems, which improves functional capacity and alleviates back pain.
- Physical activity promotes healing and reduces problems caused by back pain. The back has a strong structure and can withstand, as it gradually gets used to it, a variety of loads.

Photo: iStock






